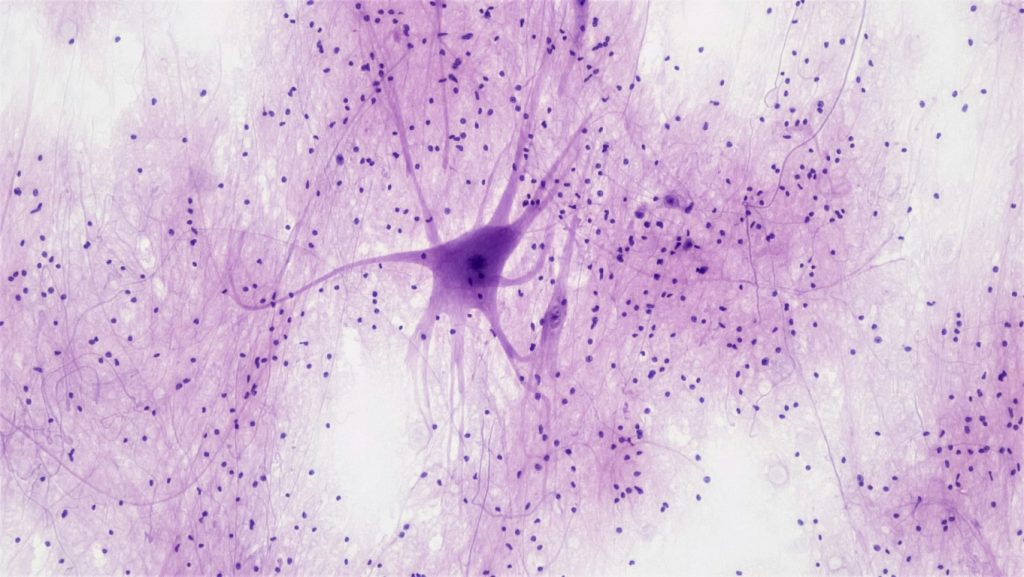
An old idea; that neurodegenerative diseases such as Alzheimer’s are linked to earlier infections such as the flu, continues to gather supporting evidence. Like football player concussions exacting a dreadful toll years later, catching the flu or Covid may make us pay a price today and tomorrow.
A new study shows correlation between short term infections, such as influenza, to future development of dementia and other neurodegenerative conditions. Richard Sima’s recent Washington Post article (“Serious dementia risk linked to infections, study shows”, October 18, 2024) summarizes the researchers’ findings.
Data used for the study is from the Baltimore Longitudinal Study of Aging (BLSA), the longest running US aging study. The authors used the BLSA to correlate serious infections, generally defined as serious enough to require a hospital visit, to blood plasma proteins, brain volume changes, and three dementia categories.
Past infections (5 years and longer) were found related to decreased brain volume and increased neurodegeneration. Three categories of neurodegeneration were examined: all dementias, Alzheimer's Disease, and vascular dementia. Other categories of neurodegeneration may be similarly linked but were represented by too few cases to be included in the study. Covid infections were also not included in this long-term study because of its short history, however, the authors stated that Covid infections and future dementia development are likely to display similar linkages.
A unique aspect of this study is the authors’ investigation of pathways that link past infections to future brain atrophy and cognitive decline. Out of 900 blood plasma proteins tested, the authors identified 35 proteins linked to brain volume changes, an indicator od dementia. Approximately 2/3’s of these proteins are pathogenic and linked to brain volume reduction. 1/3 of the remaining proteins are “protective” and linked to increased brain volume. The authors found brain protective proteins decreased and pathogenic proteins increased after infection. The combined impact of reduced protective proteins and increased pathogenic proteins results in decreasing brain volume, an indicator of dementia.
The study authors further strengthened their findings by linking infections to dementia using data from a United Kingdom aging study with nearly 500,000 subjects and a Finnish study with nearly 250,000 subjects. Infections showed similar correlation to dementia as found in the investigator’s more detailed study with the BLSA database.
Although the study doesn’t determine the cause of dementia, the authors speculate that infections shift immune system operation in a manner that reduces production of brain protective proteins while increasing production of pathogenic proteins. Protein shifts appear related to infection type (influenza, upper respiratory track, lower respiratory track, etc), which in turn, are related to volume reduction in different brain regions.
The authors conclude that serious infections should be reduced. As mentioned previously, Covid was not part of the study because of its relatively short history, however the authors state that “long Covid” may be similarly related to an infection’s impact on brain function.
The good news is that influenza, Covid and other airborne infections can be cost effectively reduced by improving fresh air ventilation. We know that doubling today’s fresh air ventilation from 20cfm/person (9.4l/s per person) to 40cfm/person (18.8l/s per person) decreases illness-related sick days by 40%, equivalent to influenza vaccination.
The authors note that vaccination against infection has combined beneficial impacts of reducing infections and reducing infection severity. Overall, we can significantly reduce infections’ short term and long-term impacts, increasing our potential for better health now and later.
Nature’s fresh air, the air we are meant to breathe, reduces airborne illness now with the bonus of helping our brains to stay healthy in future.